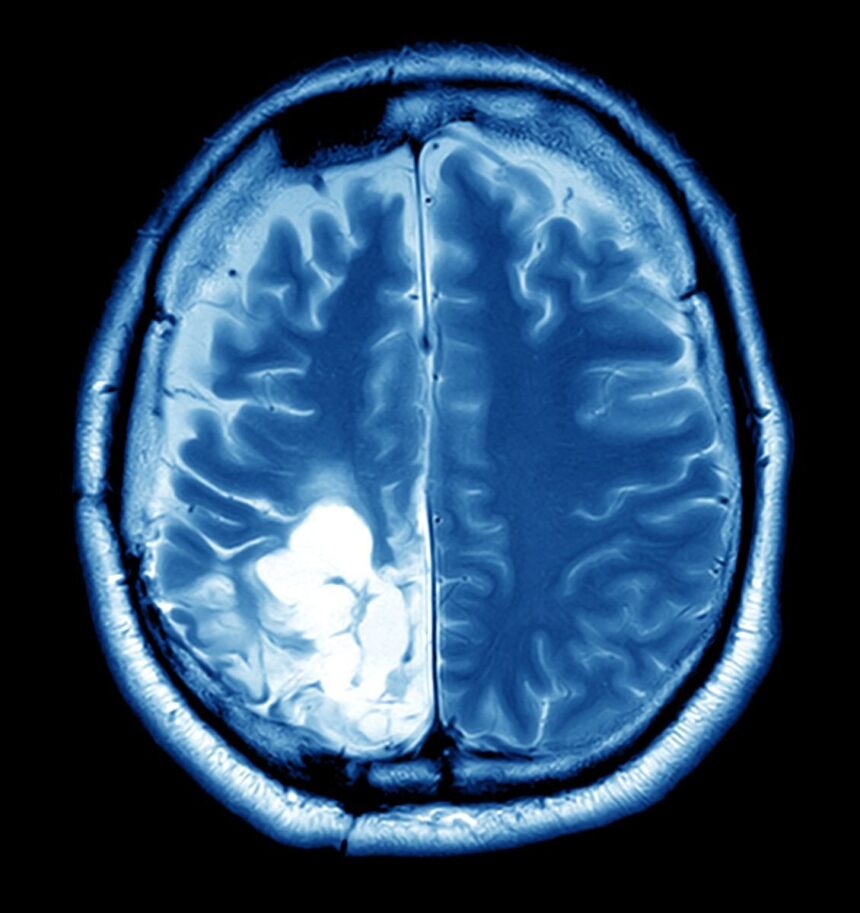
When diagnosed with a brain tumor, the therapy might seem overwhelming. Complex brain tumor treatment needs a whole-person approach that transcends expertise. This requires interdisciplinary care. Each patient’s treatment plan must satisfy a group of specialists from different professions. Radiologists, neurosurgeons, physicians, and assisted care providers must collaborate to improve patient care. Mixed care is crucial for brain tumor treatment, as explained here. This post illustrates how collaboration improves patient care and treatment.
Collaborative Team Approach
Multidisciplinary care uses cooperative teams. This is one method by which brain tumors cause numerous problems. Each team member is unique. Everyone’s contribution helps the group comprehend the patient. Neurosurgeons remove masses, while physicians treat cancer with chemotherapy and other methods. These abilities allow doctors to assess all of their patient’s health requirements and make better treatment recommendations.
Collaboration involves ongoing team communication rather than simply chatting. Regular meetings allow the team to discuss patient progress, brain tumor treatment plans, and new concerns. This dynamic conversation encourages knowledge sharing, helping practitioners stay current on research and treatment practices.
Comprehensive Treatment Planning
To build a full brain tumor treatment plan, you must understand the condition and its meaning. Modern imaging and testing capabilities let interdisciplinary teams determine the tumor’s size, location, and kind. Using this knowledge is crucial for designing a patient-specific treatment strategy. A cancer near crucial brain areas may require surgery that is different from one further away.
The brain tumor treatment strategy may vary as new information becomes available. The team regularly evaluates and adjusts the chosen approaches. Different people react differently to brain tumor therapies; therefore, this is crucial. A multidisciplinary approach that adapts to the patient’s needs helps healthcare practitioners keep treatment plans effective.
Holistic Patient Care
Multidisciplinary brain tumor treatment involves treating the complete individual, not just the brain cancer. Brain tumor diagnosis might affect mental and emotional well-being. Cancer affects both the patient and their family. In this scenario, assistance helps. The comprehensive team includes hospice, psychiatry, and social work experts who support patients during treatment.
Managing the emotional and mental effects of a brain tumor treatment is crucial to your health. Patients may feel nervous, sad, or alone throughout therapy. Mental health workers in a patient’s care team aid with these issues. Nutritionists and therapists enhance holistic treatment.
Patient Education and Empowerment
Multidisciplinary brain tumor treatment also involves patient education and independence. Patients who understand their treatment can participate more. Multidisciplinary teams prioritise communication to ensure patients and families understand the treatment strategy. Openness fosters trust and self-care.
Answering enquiries and resolving concerns empowers individuals. Since there are various specialists, patients may obtain full, personalised information. Whether discussing medication side effects or getting healthier, having access to knowledgeable specialists improves the patient experience.
Conclusion
Complex brain tumours require multidisciplinary care from a variety of specialists. These teams increase care quality and results by promoting cooperation, generating complete treatment plans, and supporting patients in all aspects of life. Knowledge and open communication empower patients and strengthen their therapeutic role. Even though brain tumour treatment is improving, a multidisciplinary approach yields the greatest outcomes.